The Delta Non Surge
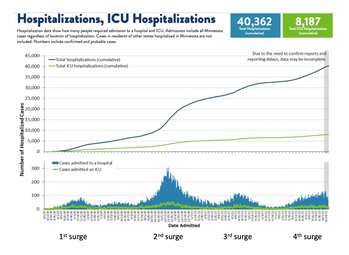
The “essential meaning” of surge, according to Merriam-Webster, is “to move very quickly and suddenly in a particular direction.” We are currently in another non-surge surge. Like the current situation, our first surge had a slow, linear, and long climb to its peak. In contrast, the first dramatic surge in New York City went up and back down in less time than our first reached the top. Our second surge last Fall/Winter was more like New York’s and the dictionary definition, quickly up and then down. Long is becoming the key word in this escalation and while the current patient numbers are fewer than last winter’s peak, this one is becoming equally as taxing due to its duration as well as fewer human resources.
Another nuance of this surge is that the highest rates of transmission are in counties outside of the metro area where vaccination rates are lower. As a result, patients are presenting at smaller, rural hospitals that don’t have the resources or critical care experience to deal with them. Normally these patients are rapidly transferred to hospitals with more capability. But with hospitals at capacity, these smaller hospitals are having to provide the best critical care they can. It’s creating significant moral stress on their providers. It’s routine for me, an intensivist, to recognize that a patient isn’t going to do well based on a constellation of comorbid conditions with COVID on top. For someone who doesn’t deal with end of life on a regular basis, seeing someone slowly deteriorate in front of your eyes is morally challenging. I received a note about a hospitalist in one of these rural hospitals managing such a patient with the help of our teleICU doc who wrote, “At first she had a lot of bravado and then eventually she started crying and said she wanted to take a leave of absence but is one of 5 hospitalists.”
I’m not sure Joe Public knows the current situation in Minnesota hospitals or what is happening to the doctors after 8 plus weeks of constantly climbing cases. I find it interesting that it was only after the New York Times had an article titled “Minnesota hospitals are nearing capacity as a virus surge batters the state” that the Minnesota media gave note and the state government leaders held a press conference at North Memorial. The Governor promised the help of the National Guard, which, as it turns out, is good at providing for space but not necessarily the shortage of personnel.
Speaking of workers, It was reported that more people quit jobs in August than since December of 2000. There are jobs everywhere. I had fast food for dinner recently and was handed a “we’re hiring” card as I entered the drive through. I couldn’t help wondering what it would be like to work without a pager. On the other hand, the fact that the manager was standing in the drive through recruiting for workers makes me think that she was experiencing equal stress. It sounds like the whole of society is ready for a leave of absence from COVID.
Jeffrey G. Chipman, MD, FACS
Frank B. Cerra Professor of Critical Care Surgery
Division Head, Critical Care, and Acute Care Surgery,
University of Minnesota
Executive Medical Director, Critical Care Domain, M Health Fairview